よむ、つかう、まなぶ。
慶應義塾大学 岸本特任教授 御提出資料 (7 ページ)
出典
| 公開元URL | https://www8.cao.go.jp/kisei-kaikaku/kisei/meeting/wg/2310_04medical/231218/medical04_agenda.html |
| 出典情報 | 規制改革推進会議 健康・医療・介護ワーキング・グループ(第4回 12/18)《内閣府》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
Psychiatry and
Clinical Neurosciences
psychiatrists remotely using their smartphones and other devices from
home. The fact that two-way video was determined noninferior to
face-to-face treatment in this study is an important finding, given that
this type of health care will continue to be used around the world.
Another important aspect of this trial is that it is the first pragmatic two-way video trial in Japan, a country with universal health
insurance where people can choose their preferred medical facilities
and receive medical care at a relatively low cost. The flip side to low
health care prices is the extremely busy treatment environment where
health care providers have to see many patients in a short period of
time. There was some concern that two-way video treatment would be
difficult to implement in such an environment. Since Japan is considered a relatively restrictive country for telemedicine,3,13 it was important to verify that two-way video treatment is equally effective in light
of existing individual and cultural regulatory environments in order to
appropriately promote its use.
The results of this study are consistent with those of previous
meta-analyses that have reported comparable efficacies of two-way
video and face-to-face treatment.9,37,38 In the evaluation of the primary outcome, treatment via two-way video was noninferior to faceto-face treatment. Although the difference did not reach significance,
numerically, the SF-36 MCS was higher in the two-way video group
at 24 weeks. There were no significant differences between the two
groups on the gold standard rating scales for each disease. The only
exception was that the HAMD score at 12 weeks for patients with
depression was significantly higher in the two-way video group than
in the face-to-face group. The reason for this is unclear, but both psychiatrists and patients may have been unfamiliar with two-way video
and may have had some difficulty with the initial treatment. However,
the baseline HAMD score of the face-to-face group was originally
higher than that of the two-way video group at the trend level, and
the difference may have been significant only incidentally. At the final
24-week time point, the significant difference between the two groups
disappeared. This study had a low dropout rate, and there were no differences between the two groups in terms of measures related to treatment alliance, such as the WAI and CSQ scores. Reflecting such
patients’ positive attitudes toward two-way video, the percentage of
two-way video use was relatively high. In this study, the two-way
video group was supposed to use two-way video for more than 50%
of visits, but the average rate of two-way video use after baseline was
approximately 77%. Furthermore, approximately one-third of patients
in the two-way video group received only two-way video treatment,
demonstrating the noninferiority of two-way video compared with
face-to-face treatment in this group as well. At the same time, the
reasons for not using two-way video 100% of the time should have
been examined in detail. This study did not collect detailed data on
the reasons why the two-way video group chose face-to-face care for
some visits, and this is an issue for future studies.
As expected, two-way video was also found to reduce the burden
of hospital visits for the patients; patients in the two-way video group
spent less time in hospital visits and had fewer expenses than patients
in the face-to-face group. The value that telemedicine can provide to
patients is significant, not to mention the time and cost-savings associated with hospital visits. These include the provision of medical
care in medically underserved areas, access to highly specialized
psychiatrists, and easier access for patients who may have difficulty
seeing a psychiatrist due to symptoms and/or stigma.
The following limitations of this study should be noted. First, we
targeted only three disorder groups, namely depressive disorders,
anxiety disorders, and OCD and related disorders. Although the three
disorder groups considered in this study can be assumed to represent
a large number of patients in psychiatric outpatient clinics, they do
not cover all psychiatric disorders, such as schizophrenia, bipolar disorder, substance-related disorder, and neurodevelopmental disorder.
Thus, a comparison between two-way video and face-to-face treatment for diseases not covered in this study remains a subject for
future research. Second, it was not possible to blind psychiatrists or
patients in this study comparing two-way video to face-to-face.
Psychiatry and Clinical Neurosciences
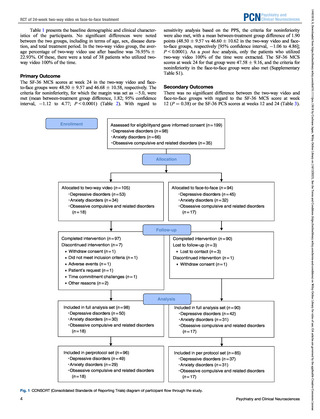
RCT of 24-week two-way video vs face-to-face treatment
However, our study implemented a centralized rating, and we were
able to implement blinding of the raters who performed the HAMD,
HAMA, and YBOCS assessments. This is part of the design advantage of this study over other studies, but, despite this, it cannot be
ruled out that the fact that physicians as well as patients knew the
assignments may have worked in favor of telemedicine when, for
example, expectations for telemedicine were high. Third, although the
present study followed patients for a relatively long period
(6 months), there is still room for further evaluation of the effects over
even longer follow-up periods, as psychiatric disorders often have a
long course. While long-term use of two-way video is likely to reduce
the financial burden on patients, it may take longer to establish a good
rapport or reduce the quality of an established rapport, compared with
face-to-face treatment.39 Future research should examine the usefulness of two-way video for longer periods of time and the desirable
methods of operation.
Conclusion
The study showed that two-way video treatment over a 6-month
period was no less effective than face-to-face treatment in patients
with depressive disorders, anxiety disorders, OCD and related disorders. Many of the patients accessed their psychiatrists from home
using smartphones, which is meaningful in that the study demonstrated the effectiveness of a modern form of telemedicine. In addition, this was the first RCT conducted in a real-world clinical setting
in Japan, and the results indicate that two-way video is a practical
option in Japan and can be used equally with face-to-face treatment.
In future studies, longer follow-up and further validation of the usefulness of disease-specific two-way video treatment will be desirable.
Acknowledgments
The authors are grateful to the other members of J-PROTECT
(Japanese Project for Telepsychiatry Evaluation During COVID-19:
Treatment Comparison Trial) collaborators: Dr Kazunari Yoshida, Dr
Toshiro Horigome, Dr Mayu Fujikawa, Ms Kumiko Hiza, Ms Hiromi
Mikami, M. Saki Hattori, Mr Masao Takaishi, Mr Satoshi Tsujimura,
Mr Hajime Tamura, Ms Junko Suzuki, Ms Keiko Komiyada, Dr Anri
Watanabe, Dr Yoshihiro Matsumoto, Ms Satoko Kimura, Ms Haruka
Okamoto, Dr Kyosuke Sawada, Ms Yuka Oba, Mr Satoshi Tsujimura,
Ms Shii Sagae, Mr Kiyoji Nagao, Mr Ryuhei Terashi, Ms Sumako
Onishi, Ms Mayumi Hiruma, Ms Junko Kannari, Ms Kanako Sasao,
Ms Ayumi Konishi, Ms Nobuko Haga, Mr Nobuhiko Noguchi, Mr
Kosuke Hino, Mr Yuya Igarashi, and Dr Takaharu Azekawa for their
support with designing the study, data collection, and management
protocols used in this study. The authors would like to express their
sincere gratitude to the late Dr. Yoshinori Watanabe for his invaluable
help in conducting the study.
Disclosure statement
The authors declare the following financial interests/personal relationships that may be considered as potential competing interests:
Taishiro Kishimoto has received grants from Sumitomo, Otsuka, and
Micin; royalties or licenses from Sumitomo and FRONTEO; consulting fees from TechDoctor and FRONTEO; speaker’s honoraria from
Sumitomo, Boehringer Ingelheim, Takeda, Astellas, Meiji Seika, and
Janssen; and stock from i2medical and TechDoctor. Takeshi Asami
has received speaker’s honoraria from Otsuka, Meiji Seika,
Sumitomo, Lundbeck, Yoshitomiyakuhin, Eisai, MSD, and Takeda;
and scholarship grants from Otsuka and PDRadiopharma. Akira Suda
has received grants from Otsuka; speaker’s honoraria from Eisai,
Lundbeck, Meiji Seika, MSD K.K., and Takeda. Toshiaki Kikuchi
has received speaker’s honoraria from Takeda, Lundbeck, Viatris,
Sumitomo, and MSD. Mitsuhiro Sado has received research support
from the Japan Research Institute; royalties from Igaku-Shoin, SeiwaShoten, Sogensha, and Kongo-Shuppan; and lecture fees from
Mochida, Takeda, Sumitomo, and Viatris. Masaru Mimura has
received grants from Daiichi Sankyo, Eisai, FRONTEO, Shionogi,
7
14401819, 0, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/pcn.13618 by Cochrane Japan, Wiley Online Library on [16/12/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
PCN
Clinical Neurosciences
psychiatrists remotely using their smartphones and other devices from
home. The fact that two-way video was determined noninferior to
face-to-face treatment in this study is an important finding, given that
this type of health care will continue to be used around the world.
Another important aspect of this trial is that it is the first pragmatic two-way video trial in Japan, a country with universal health
insurance where people can choose their preferred medical facilities
and receive medical care at a relatively low cost. The flip side to low
health care prices is the extremely busy treatment environment where
health care providers have to see many patients in a short period of
time. There was some concern that two-way video treatment would be
difficult to implement in such an environment. Since Japan is considered a relatively restrictive country for telemedicine,3,13 it was important to verify that two-way video treatment is equally effective in light
of existing individual and cultural regulatory environments in order to
appropriately promote its use.
The results of this study are consistent with those of previous
meta-analyses that have reported comparable efficacies of two-way
video and face-to-face treatment.9,37,38 In the evaluation of the primary outcome, treatment via two-way video was noninferior to faceto-face treatment. Although the difference did not reach significance,
numerically, the SF-36 MCS was higher in the two-way video group
at 24 weeks. There were no significant differences between the two
groups on the gold standard rating scales for each disease. The only
exception was that the HAMD score at 12 weeks for patients with
depression was significantly higher in the two-way video group than
in the face-to-face group. The reason for this is unclear, but both psychiatrists and patients may have been unfamiliar with two-way video
and may have had some difficulty with the initial treatment. However,
the baseline HAMD score of the face-to-face group was originally
higher than that of the two-way video group at the trend level, and
the difference may have been significant only incidentally. At the final
24-week time point, the significant difference between the two groups
disappeared. This study had a low dropout rate, and there were no differences between the two groups in terms of measures related to treatment alliance, such as the WAI and CSQ scores. Reflecting such
patients’ positive attitudes toward two-way video, the percentage of
two-way video use was relatively high. In this study, the two-way
video group was supposed to use two-way video for more than 50%
of visits, but the average rate of two-way video use after baseline was
approximately 77%. Furthermore, approximately one-third of patients
in the two-way video group received only two-way video treatment,
demonstrating the noninferiority of two-way video compared with
face-to-face treatment in this group as well. At the same time, the
reasons for not using two-way video 100% of the time should have
been examined in detail. This study did not collect detailed data on
the reasons why the two-way video group chose face-to-face care for
some visits, and this is an issue for future studies.
As expected, two-way video was also found to reduce the burden
of hospital visits for the patients; patients in the two-way video group
spent less time in hospital visits and had fewer expenses than patients
in the face-to-face group. The value that telemedicine can provide to
patients is significant, not to mention the time and cost-savings associated with hospital visits. These include the provision of medical
care in medically underserved areas, access to highly specialized
psychiatrists, and easier access for patients who may have difficulty
seeing a psychiatrist due to symptoms and/or stigma.
The following limitations of this study should be noted. First, we
targeted only three disorder groups, namely depressive disorders,
anxiety disorders, and OCD and related disorders. Although the three
disorder groups considered in this study can be assumed to represent
a large number of patients in psychiatric outpatient clinics, they do
not cover all psychiatric disorders, such as schizophrenia, bipolar disorder, substance-related disorder, and neurodevelopmental disorder.
Thus, a comparison between two-way video and face-to-face treatment for diseases not covered in this study remains a subject for
future research. Second, it was not possible to blind psychiatrists or
patients in this study comparing two-way video to face-to-face.
Psychiatry and Clinical Neurosciences
RCT of 24-week two-way video vs face-to-face treatment
However, our study implemented a centralized rating, and we were
able to implement blinding of the raters who performed the HAMD,
HAMA, and YBOCS assessments. This is part of the design advantage of this study over other studies, but, despite this, it cannot be
ruled out that the fact that physicians as well as patients knew the
assignments may have worked in favor of telemedicine when, for
example, expectations for telemedicine were high. Third, although the
present study followed patients for a relatively long period
(6 months), there is still room for further evaluation of the effects over
even longer follow-up periods, as psychiatric disorders often have a
long course. While long-term use of two-way video is likely to reduce
the financial burden on patients, it may take longer to establish a good
rapport or reduce the quality of an established rapport, compared with
face-to-face treatment.39 Future research should examine the usefulness of two-way video for longer periods of time and the desirable
methods of operation.
Conclusion
The study showed that two-way video treatment over a 6-month
period was no less effective than face-to-face treatment in patients
with depressive disorders, anxiety disorders, OCD and related disorders. Many of the patients accessed their psychiatrists from home
using smartphones, which is meaningful in that the study demonstrated the effectiveness of a modern form of telemedicine. In addition, this was the first RCT conducted in a real-world clinical setting
in Japan, and the results indicate that two-way video is a practical
option in Japan and can be used equally with face-to-face treatment.
In future studies, longer follow-up and further validation of the usefulness of disease-specific two-way video treatment will be desirable.
Acknowledgments
The authors are grateful to the other members of J-PROTECT
(Japanese Project for Telepsychiatry Evaluation During COVID-19:
Treatment Comparison Trial) collaborators: Dr Kazunari Yoshida, Dr
Toshiro Horigome, Dr Mayu Fujikawa, Ms Kumiko Hiza, Ms Hiromi
Mikami, M. Saki Hattori, Mr Masao Takaishi, Mr Satoshi Tsujimura,
Mr Hajime Tamura, Ms Junko Suzuki, Ms Keiko Komiyada, Dr Anri
Watanabe, Dr Yoshihiro Matsumoto, Ms Satoko Kimura, Ms Haruka
Okamoto, Dr Kyosuke Sawada, Ms Yuka Oba, Mr Satoshi Tsujimura,
Ms Shii Sagae, Mr Kiyoji Nagao, Mr Ryuhei Terashi, Ms Sumako
Onishi, Ms Mayumi Hiruma, Ms Junko Kannari, Ms Kanako Sasao,
Ms Ayumi Konishi, Ms Nobuko Haga, Mr Nobuhiko Noguchi, Mr
Kosuke Hino, Mr Yuya Igarashi, and Dr Takaharu Azekawa for their
support with designing the study, data collection, and management
protocols used in this study. The authors would like to express their
sincere gratitude to the late Dr. Yoshinori Watanabe for his invaluable
help in conducting the study.
Disclosure statement
The authors declare the following financial interests/personal relationships that may be considered as potential competing interests:
Taishiro Kishimoto has received grants from Sumitomo, Otsuka, and
Micin; royalties or licenses from Sumitomo and FRONTEO; consulting fees from TechDoctor and FRONTEO; speaker’s honoraria from
Sumitomo, Boehringer Ingelheim, Takeda, Astellas, Meiji Seika, and
Janssen; and stock from i2medical and TechDoctor. Takeshi Asami
has received speaker’s honoraria from Otsuka, Meiji Seika,
Sumitomo, Lundbeck, Yoshitomiyakuhin, Eisai, MSD, and Takeda;
and scholarship grants from Otsuka and PDRadiopharma. Akira Suda
has received grants from Otsuka; speaker’s honoraria from Eisai,
Lundbeck, Meiji Seika, MSD K.K., and Takeda. Toshiaki Kikuchi
has received speaker’s honoraria from Takeda, Lundbeck, Viatris,
Sumitomo, and MSD. Mitsuhiro Sado has received research support
from the Japan Research Institute; royalties from Igaku-Shoin, SeiwaShoten, Sogensha, and Kongo-Shuppan; and lecture fees from
Mochida, Takeda, Sumitomo, and Viatris. Masaru Mimura has
received grants from Daiichi Sankyo, Eisai, FRONTEO, Shionogi,
7
14401819, 0, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/pcn.13618 by Cochrane Japan, Wiley Online Library on [16/12/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
PCN