よむ、つかう、まなぶ。
慶應義塾大学 岸本特任教授 御提出資料 (8 ページ)
出典
| 公開元URL | https://www8.cao.go.jp/kisei-kaikaku/kisei/meeting/wg/2310_04medical/231218/medical04_agenda.html |
| 出典情報 | 規制改革推進会議 健康・医療・介護ワーキング・グループ(第4回 12/18)《内閣府》 |
ページ画像
ダウンロードした画像を利用する際は「出典情報」を明記してください。
低解像度画像をダウンロード
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
Takeda, Tanabe Mitsubishi, and Tsumura; speaker’s honoraria from
Biogen Japan, Byer Pharmaceutical, Daiichi Sankyo, Sumitomo
Pharma, Demant Japan, Eisai, Eli Lilly, Fuji Film RI Pharma,
Hisamitsu, H.U. Frontier, Janssen, Mochida, MSD, Mylan EPD,
Nippon Chemiphar, Novartis, Ono Yakuhin, Otsuka, Pfizer, Shionogi,
Takeda, Teijin, and Viatris. Kengo Nagashima has received consulting fees from SENJU, Toray, and Kowa. Takashi Nakamae has
received a telemedicine system from Medley, and speaker’s honoraria
from AstraZeneca and Lundbeck. Yoshinari Abe has received a telemedicine system from Medley. Tetsufumi Kanazawa has received
speaker’s honoraria from EA Pharma Co., Ltd., Eisai Co., Ltd.,
Janssen Pharmaceutical K.K., Lundbeck, Meiji Seika Pharma Co.,
Ltd., MSD K.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc.,
Sumitomo Dainippon Pharma Co., Ltd., Takeda Pharmaceutical
Company Limited, and Viatris Inc.; received grants from Eisai Co.,
Ltd., Otsuka Pharmaceutical Co., Ltd., and Sumitomo Dainippon
Pharma Co., Ltd.; and received a supervision fee for advertising
materials from Teijin-Pharma Co., Ltd. Hiroaki Tomita has received
grants from Daiichi-Sankyo, Eisai, Otsuka, and Sumitomo Pharma;
speaker’s honoraria from Daiichi-Sankyo, EA Pharma, Eisai, Janssen,
Lundbeck, Meiji Seika, Mochida, MSD, Mylan EPD, Otsuka, Pfizer,
Sumitomo Pharma, Takeda, and Viatris. Hiroshi Kimura has received
speaker’s honoraria from Otsuka, Meiji Seika, Janssen, Teijin,
Takeda, MSD, and Sumitomo pharma. Aiko Sato has received
speaker’s honoraria from Takeda and Lundbeck. Naoya Sugiyama has
received consulting fees from Hisamitsu, and speaker’s honoraria
from Sumitomo, Otsuka, Janssen, UCB, Shionogi, EA, Eisai, and
Viatris. Masaru Mimura is a vice editor in chief of Psychiatry
and Clinical Neurosciences and a co-author of this article. Hiroaki
Tomita is an editorial board member of Psychiatry and Clinical Neurosciences and a co-author of this article. To minimize bias, they were
excluded from all editorial decision-making related to the acceptance
of this article for publication.
Author contributions
All authors were involved in designing the study. Akitoyo Hishimoto,
Takeshi Asami, Akira Suda, Shogyoku Bun, Toshiaki Kikuchi,
Akihiro Takamiya, Takashi Nakamae, Yoshinari Abe, Tetsufumi
Kanazawa, Yasuo Kawabata, Hiroaki Tomita, Koichi Abe, Seiji
Hongo, Hiroshi Kimura, Aiko Sato, Hisashi Kida, Kei Sakuma,
Michitaka Funayama, Naoya Sugiyama, Kousuke Hino, Toru
Amagai, Maki Takamiya, Hideyuki Kodama, Kenichi Goto, and
Shuichiro Fujiwara contributed to the recruiting of patients and
collecting the data. Yasunori Sato, Ryo Takemura, and Kengo
Nagashima analyzed the data. Taishiro Kishimoto and Shotaro
Kinoshita prepared the original draft. All authors contributed to the
final draft. All authors have read and approved the final manuscript.
Funding Information
This research is supported by the Japan Agency for Medical Research
and Development (AMED) under grant number JP22dk0307098. The
funding source did not participate in the design of this study and did
not have any hand in the study’s execution, analyses, or submission of
results.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
References
1.
2.
3.
4.
8
World Health Organization. Telemedicine: Opportunities and Developments in Member States. Report on the second global survey on eHealth.
World Health Organization, Genève, 2010.
World Health Organization. The Impact of COVID-19 on Mental,
Neurological and Substance Use Services: Results of a Rapid
Assessment. 2020.
Kinoshita S, Cortright K, Crawford A et al. Changes in telepsychiatry
regulations during the COVID-19 pandemic: 17 countries and regions’
approaches to an evolving healthcare landscape. Psychol. Med. 2022; 52:
2606–2613.
Zangani C, Ostinelli EG, Smith KA et al. Impact of the COVID-19
pandemic on the global delivery of mental health services and telemental
health: Systematic review. JMIR Mental Health 2022; 9: e38600.
26.
27.
28.
29.
30.
Psychiatry and
Clinical Neurosciences
Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ,
Yellowlees PM. The effectiveness of telemental health: A 2013 review.
Telemedicine and e-Health 2013; 19: 444–454.
Salmoiraghi A, Hussain S. A systematic review of the use of
telepsychiatry in acute settings. J. Psychiatr. Pract. 2015; 21: 389–393.
Basit SA, Mathews N, Kunik ME. Telemedicine interventions for
medication adherence in mental illness: A systematic review. Gen. Hosp.
Psychiatry 2020; 62: 28–36.
Guaiana G, Mastrangelo J, Hendrikx S, Barbui C. A systematic review
of the use of telepsychiatry in depression. Community Ment. Health J.
2021; 57: 93–100.
Hagi K, Kurokawa S, Takamiya A, Fujikawa M, Kinoshita S,
Kishimoto T. Telepsychiatry versus face–to–face treatment: A systematic
review and meta-analysis of randomized controlled trials. Br.
J. Psychiatry 2023; 223: 407–414.
De Las CC, Arredondo MT, Cabrera MF, Sulzenbacher H, Meise U.
Randomized clinical trial of telepsychiatry through videoconference
versus face-to-face conventional psychiatric treatment. Telemedicine
Journal & e-Health 2006; 12: 341–350.
O’Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is
telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr. Serv. 2007; 58: 836–843.
Stubbings DR, Rees CS, Roberts LD, Kane RT. Comparing in-person to
videoconference-based cognitive behavioral therapy for mood and anxiety disorders: Randomized controlled trial. J. Med. Internet Res. 2013;
15: e258.
Kinoshita S, Kishimoto T. Current status and challenges of the dissemination of telemedicine in Japan after the start of the COVID-19
pandemic. Telemedicine and e-Health 2022; 28: 1220–1224.
Kinoshita A, Kishimoto T. The use of a national identification system to
prevent misuse of benzodiazepines and Z-drugs in Japan. Lancet Psychiatry
2023; 10: e26.
Ministry of Health, Labour and Welfare. Q&A on the Temporary
and Exceptional Treatment of Medical Treatment Using Telephones
and Information and Communication Devices during the Spread of New
Coronavirus Infections. 2020. https://www.mhlw.go.jp/content/000627376.pdf.
Kinoshita S. The diffusion and challenges of telemedicine in the
with/after COVID-19 era. Journal of Information and Communications
Policy 2021; 5: 49–67.
Ikegami N, Yoo BK, Hashimoto H et al. Japanese universal health coverage:
Evolution, achievements, and challenges. The Lancet 2011; 378: 1106–1115.
Hiyama T, Yoshihara M. New occupational threats to Japanese physicians: Karoshi (death due to overwork) and karojisatsu (suicide due to
overwork). Occup. Environ. Med. 2008; 65: 428–429.
Kinoshita S, Kishimoto T. Decline in Japan’s research capabilities: Challenges in the medical field. The Lancet 2023; 402: 1239–1240.
Kishimoto T, Kinoshita S, Bun S et al. Japanese Project for
Telepsychiatry Evaluation During COVID-19: Treatment Comparison
Trial (J-PROTECT): Rationale, design, and methodology. Contemp. Clin.
Trials 2021; 111: 106596.
DSM-5 American Psychiatric Association. Diagnostic and Statistical
Manual of Mental Disorders. American Psychiatric Publishing,
Arlington, 2013; 10.
Efron B. Forcing a sequential experiment to be balanced. Biometrika
1971; 58: 403–417.
Ware JE, Kosinski M, Keller S. SF-36 physical and mental health
summary scales. A user’s Manual 2001; 1994.
Horvath AO, Greenberg LS. Development and validation of the working
Alliance inventory. J. Couns. Psychol. 1989; 36: 223–233.
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of
client/patient satisfaction: Development of a general scale. Eval. Program
Plann. 1979; 2: 197–207.
Brooks R, Group E. EuroQol: The current state of play. Health Policy
1996; 37: 53–72.
Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960; 23: 56–62.
Hamilton MAX. The assessment of anxiety states by rating. British
Journal of Medical Psychology. 1959; 32: 50–55.
Goodman WK, Price LH, Rasmussen SA et al. The Yale-Brown
obsessive compulsive scale: I. Development, use, and reliability. Arch.
Gen. Psychiatry 1989; 46: 1006–1011.
Fortney JC, Pyne JM, Mouden SB et al. Practice-based versus
telemedicine-based collaborative care for depression in rural federally
qualified health centers: A pragmatic randomized comparative effectiveness trial. Am. J. Psychiatry 2013; 170: 414–425.
Psychiatry and Clinical Neurosciences
14401819, 0, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/pcn.13618 by Cochrane Japan, Wiley Online Library on [16/12/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
PCN
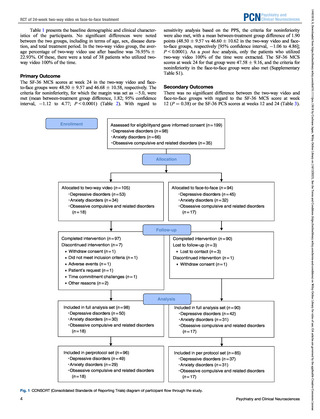
RCT of 24-week two-way video vs face-to-face treatment
Biogen Japan, Byer Pharmaceutical, Daiichi Sankyo, Sumitomo
Pharma, Demant Japan, Eisai, Eli Lilly, Fuji Film RI Pharma,
Hisamitsu, H.U. Frontier, Janssen, Mochida, MSD, Mylan EPD,
Nippon Chemiphar, Novartis, Ono Yakuhin, Otsuka, Pfizer, Shionogi,
Takeda, Teijin, and Viatris. Kengo Nagashima has received consulting fees from SENJU, Toray, and Kowa. Takashi Nakamae has
received a telemedicine system from Medley, and speaker’s honoraria
from AstraZeneca and Lundbeck. Yoshinari Abe has received a telemedicine system from Medley. Tetsufumi Kanazawa has received
speaker’s honoraria from EA Pharma Co., Ltd., Eisai Co., Ltd.,
Janssen Pharmaceutical K.K., Lundbeck, Meiji Seika Pharma Co.,
Ltd., MSD K.K., Otsuka Pharmaceutical Co., Ltd., Pfizer Japan Inc.,
Sumitomo Dainippon Pharma Co., Ltd., Takeda Pharmaceutical
Company Limited, and Viatris Inc.; received grants from Eisai Co.,
Ltd., Otsuka Pharmaceutical Co., Ltd., and Sumitomo Dainippon
Pharma Co., Ltd.; and received a supervision fee for advertising
materials from Teijin-Pharma Co., Ltd. Hiroaki Tomita has received
grants from Daiichi-Sankyo, Eisai, Otsuka, and Sumitomo Pharma;
speaker’s honoraria from Daiichi-Sankyo, EA Pharma, Eisai, Janssen,
Lundbeck, Meiji Seika, Mochida, MSD, Mylan EPD, Otsuka, Pfizer,
Sumitomo Pharma, Takeda, and Viatris. Hiroshi Kimura has received
speaker’s honoraria from Otsuka, Meiji Seika, Janssen, Teijin,
Takeda, MSD, and Sumitomo pharma. Aiko Sato has received
speaker’s honoraria from Takeda and Lundbeck. Naoya Sugiyama has
received consulting fees from Hisamitsu, and speaker’s honoraria
from Sumitomo, Otsuka, Janssen, UCB, Shionogi, EA, Eisai, and
Viatris. Masaru Mimura is a vice editor in chief of Psychiatry
and Clinical Neurosciences and a co-author of this article. Hiroaki
Tomita is an editorial board member of Psychiatry and Clinical Neurosciences and a co-author of this article. To minimize bias, they were
excluded from all editorial decision-making related to the acceptance
of this article for publication.
Author contributions
All authors were involved in designing the study. Akitoyo Hishimoto,
Takeshi Asami, Akira Suda, Shogyoku Bun, Toshiaki Kikuchi,
Akihiro Takamiya, Takashi Nakamae, Yoshinari Abe, Tetsufumi
Kanazawa, Yasuo Kawabata, Hiroaki Tomita, Koichi Abe, Seiji
Hongo, Hiroshi Kimura, Aiko Sato, Hisashi Kida, Kei Sakuma,
Michitaka Funayama, Naoya Sugiyama, Kousuke Hino, Toru
Amagai, Maki Takamiya, Hideyuki Kodama, Kenichi Goto, and
Shuichiro Fujiwara contributed to the recruiting of patients and
collecting the data. Yasunori Sato, Ryo Takemura, and Kengo
Nagashima analyzed the data. Taishiro Kishimoto and Shotaro
Kinoshita prepared the original draft. All authors contributed to the
final draft. All authors have read and approved the final manuscript.
Funding Information
This research is supported by the Japan Agency for Medical Research
and Development (AMED) under grant number JP22dk0307098. The
funding source did not participate in the design of this study and did
not have any hand in the study’s execution, analyses, or submission of
results.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
References
1.
2.
3.
4.
8
World Health Organization. Telemedicine: Opportunities and Developments in Member States. Report on the second global survey on eHealth.
World Health Organization, Genève, 2010.
World Health Organization. The Impact of COVID-19 on Mental,
Neurological and Substance Use Services: Results of a Rapid
Assessment. 2020.
Kinoshita S, Cortright K, Crawford A et al. Changes in telepsychiatry
regulations during the COVID-19 pandemic: 17 countries and regions’
approaches to an evolving healthcare landscape. Psychol. Med. 2022; 52:
2606–2613.
Zangani C, Ostinelli EG, Smith KA et al. Impact of the COVID-19
pandemic on the global delivery of mental health services and telemental
health: Systematic review. JMIR Mental Health 2022; 9: e38600.
26.
27.
28.
29.
30.
Psychiatry and
Clinical Neurosciences
Hilty DM, Ferrer DC, Parish MB, Johnston B, Callahan EJ,
Yellowlees PM. The effectiveness of telemental health: A 2013 review.
Telemedicine and e-Health 2013; 19: 444–454.
Salmoiraghi A, Hussain S. A systematic review of the use of
telepsychiatry in acute settings. J. Psychiatr. Pract. 2015; 21: 389–393.
Basit SA, Mathews N, Kunik ME. Telemedicine interventions for
medication adherence in mental illness: A systematic review. Gen. Hosp.
Psychiatry 2020; 62: 28–36.
Guaiana G, Mastrangelo J, Hendrikx S, Barbui C. A systematic review
of the use of telepsychiatry in depression. Community Ment. Health J.
2021; 57: 93–100.
Hagi K, Kurokawa S, Takamiya A, Fujikawa M, Kinoshita S,
Kishimoto T. Telepsychiatry versus face–to–face treatment: A systematic
review and meta-analysis of randomized controlled trials. Br.
J. Psychiatry 2023; 223: 407–414.
De Las CC, Arredondo MT, Cabrera MF, Sulzenbacher H, Meise U.
Randomized clinical trial of telepsychiatry through videoconference
versus face-to-face conventional psychiatric treatment. Telemedicine
Journal & e-Health 2006; 12: 341–350.
O’Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is
telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr. Serv. 2007; 58: 836–843.
Stubbings DR, Rees CS, Roberts LD, Kane RT. Comparing in-person to
videoconference-based cognitive behavioral therapy for mood and anxiety disorders: Randomized controlled trial. J. Med. Internet Res. 2013;
15: e258.
Kinoshita S, Kishimoto T. Current status and challenges of the dissemination of telemedicine in Japan after the start of the COVID-19
pandemic. Telemedicine and e-Health 2022; 28: 1220–1224.
Kinoshita A, Kishimoto T. The use of a national identification system to
prevent misuse of benzodiazepines and Z-drugs in Japan. Lancet Psychiatry
2023; 10: e26.
Ministry of Health, Labour and Welfare. Q&A on the Temporary
and Exceptional Treatment of Medical Treatment Using Telephones
and Information and Communication Devices during the Spread of New
Coronavirus Infections. 2020. https://www.mhlw.go.jp/content/000627376.pdf.
Kinoshita S. The diffusion and challenges of telemedicine in the
with/after COVID-19 era. Journal of Information and Communications
Policy 2021; 5: 49–67.
Ikegami N, Yoo BK, Hashimoto H et al. Japanese universal health coverage:
Evolution, achievements, and challenges. The Lancet 2011; 378: 1106–1115.
Hiyama T, Yoshihara M. New occupational threats to Japanese physicians: Karoshi (death due to overwork) and karojisatsu (suicide due to
overwork). Occup. Environ. Med. 2008; 65: 428–429.
Kinoshita S, Kishimoto T. Decline in Japan’s research capabilities: Challenges in the medical field. The Lancet 2023; 402: 1239–1240.
Kishimoto T, Kinoshita S, Bun S et al. Japanese Project for
Telepsychiatry Evaluation During COVID-19: Treatment Comparison
Trial (J-PROTECT): Rationale, design, and methodology. Contemp. Clin.
Trials 2021; 111: 106596.
DSM-5 American Psychiatric Association. Diagnostic and Statistical
Manual of Mental Disorders. American Psychiatric Publishing,
Arlington, 2013; 10.
Efron B. Forcing a sequential experiment to be balanced. Biometrika
1971; 58: 403–417.
Ware JE, Kosinski M, Keller S. SF-36 physical and mental health
summary scales. A user’s Manual 2001; 1994.
Horvath AO, Greenberg LS. Development and validation of the working
Alliance inventory. J. Couns. Psychol. 1989; 36: 223–233.
Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD. Assessment of
client/patient satisfaction: Development of a general scale. Eval. Program
Plann. 1979; 2: 197–207.
Brooks R, Group E. EuroQol: The current state of play. Health Policy
1996; 37: 53–72.
Hamilton M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960; 23: 56–62.
Hamilton MAX. The assessment of anxiety states by rating. British
Journal of Medical Psychology. 1959; 32: 50–55.
Goodman WK, Price LH, Rasmussen SA et al. The Yale-Brown
obsessive compulsive scale: I. Development, use, and reliability. Arch.
Gen. Psychiatry 1989; 46: 1006–1011.
Fortney JC, Pyne JM, Mouden SB et al. Practice-based versus
telemedicine-based collaborative care for depression in rural federally
qualified health centers: A pragmatic randomized comparative effectiveness trial. Am. J. Psychiatry 2013; 170: 414–425.
Psychiatry and Clinical Neurosciences
14401819, 0, Downloaded from https://onlinelibrary.wiley.com/doi/10.1111/pcn.13618 by Cochrane Japan, Wiley Online Library on [16/12/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
PCN
RCT of 24-week two-way video vs face-to-face treatment