【参考資料4】抗微生物薬適正使用の手引き 第三版 本編 (130 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_45318.html |
| 出典情報 | 厚生科学審議会 感染症部会 薬剤耐性(AMR)に関する小委員会 抗微生物薬適正使用(AMS)等に関する作業部会(第6回 11/19)《厚生労働省》 |
ページ画像
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
第三版
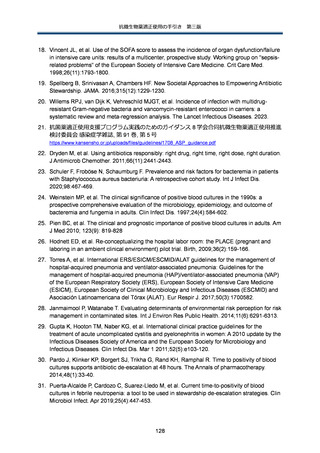
46. Garnacho-Montero J, Gutiérrez-Pizarraya A, Escoresca-Ortega A, et al. De-escalation of
empirical therapy is associated with lower mortality in patients with severe sepsis and septic
shock. Intensive Care Med. 2014 Jan;40(1):32-40.
47. Guo Y, Gao W, Yang H, Ma Ce, Sui S. De-escalation of empiric antibiotics in patients with
severe sepsis or septic shock: A meta-analysis. Heart Lung. 2016Sep-Oct;45(5):454-459.
48. Routsi C, Gkoufa A, Arvaniti K, et al. De-escalation of antimicrobial therapy in ICU settings
with high prevalence of multidrug-resistant bacteria: a multicentre prospective observational
cohort study in patients with sepsis or septic shock. J Antimicrob Chemother. 2020
Dec;75(12):3665-3674.
49. Lakbar I, De Waele JJ, Tabah A, Einav S, Martin-Loeches I, Leone M. Antimicrobial DeEscalation in the ICU: From Recommendations to Level of Evidence. Adv Ther. 2020
Jul;37(7):3083-3096.
50. Lin J, Zhou M, Chen J, Zhang L, Lu M, Liu Z. De-escalation from Echinocandins to Azole
Treatment in Critically Ill Patients with Candidemia. International journal of infectious
diseases. Int J Infect Dis. 2022 Aug;121:69-74.
51. Bailly S, Leroy O, Montravers P, et al. Antifungal de-escalation was not associated with
adverse outcome in critically ill patients treated for invasive candidiasis: post hoc analyses of
the AmarCAND2 study data. Intensive care Med. 2015 Nov;41(11):1931-1940.
52. Seddon MM, Bookstaver PB, Justo JA, et al. Role of Early De-escalation of Antimicrobial
Therapy on Risk of Clostridioides difficile Infection Following Enterobacteriaceae
Bloodstream Infections. Clin Infect Dis. 2019 Jul;69(3):414-420.
53. Lew KY, Ng TM, Tan M, et al. Safety and clinical outcomes of carbapenem de-escalation as
part of an antimicrobial stewardship programme in an ESBL-endemic setting. J Antimicrobial
Chemother. 2015 Apr;70(4):1219-1225.
54. Tagashira Y, Horiuchi M, Tokuda Y, Heist BS, Higuchi M, Honda H. Antimicrobial stewardship
for carbapenem use at a Japanese tertiary care center: An interrupted time series analysis
on the impact of infectious disease consultation, prospective audit, and feedback. Am J Infect
Control. 2016 Jun;44(6):708-710.
55. Honda H, Murakami S, Tagashira Y, et al. Efficacy of a Postprescription Review of BroadSpectrum Antimicrobial Agents With Feedback: A 4-Year Experience of Antimicrobial
Stewardship at a Tertiary Care Center. Open Forum Infect Dis. 2018 Nov;5(12):ofy314.
56. Akazawa T, Kusama Y, Fukuda H, et al. Eight-Year Experience of Antimicrobial Stewardship
Program and the Trend of Carbapenem Use at a Tertiary Acute-Care Hospital in Japan-The
Impact of Postprescription Review and Feedback. Open Forum Infect Dis. 2019
Sep;6(10):ofz389.
57. Morgan DJ, Coffey KC. Shorter Courses of Antibiotics for Urinary Tract Infection in Men.
JAMA. 2021 Jul;326(4):309-310.
58. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in
2019: a systematic analysis. Lancet. 2022 Feb;399(10325):629-655.
59. Ramirez J, et al. Antibiotics as Major Disruptors of Gut Microbiota. Front Cell Infect Microbiol.
2020 Nov;10:572912.
60. Esaiassen E, et al. Antibiotic exposure in neonates and early adverse outcomes: a
systematic review and meta-analysis. J Antimicrob Chemother. 2017 Jul;72(7):1858-1870,
130