参考資料1-1_長時間労働医師への健康確保措置に関するマニュアル(改訂版) (70 ページ)
出典
| 公開元URL | https://www.mhlw.go.jp/stf/newpage_35532.html |
| 出典情報 | 医師の働き方改革の推進に関する検討会(第18回 10/12)《厚生労働省》 |
ページ画像
プレーンテキスト
資料テキストはコンピュータによる自動処理で生成されており、完全に資料と一致しない場合があります。
テキストをコピーしてご利用いただく際は資料と付け合わせてご確認ください。
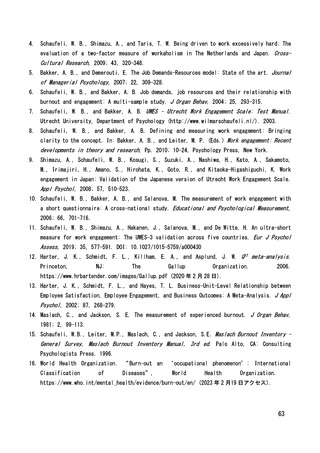
90, 484-492.
33. Solms L, van Vianen AEM, Theeboom T, et al. Keep the fire burning: a survey study on the
role of personal resources for work engagement and burnout in medical residents and
specialists in the Netherlands. BMJ Open. 2019;9:e031053. doi:10.1136/bmjopen-2019-031053
34. Yang S, Huang H, Qiu T, et al. Psychological capital mediates the association between
perceived organizational support and work engagement among Chinese doctors. Front Pub
Health. 2020;8. doi:10.3389/fpubh.2020.00149
35. Roll M, Canham L, Salamh P, Covington K, Simon C, Cook C. A novel tool for evaluating noncognitive traits of doctor of physical therapy learners in the United States. J Educ Eval
Health Prof. 2018;15. doi:10.3352/jeehp.2018.15.19
36. Macaron MM, Segun-Omosehin OA, Matar RH, Beran A, Nakanishi H, Than CA, Abulseoud, OA. A
systematic review and meta analysis on burnout in physicians during the COVID-19 pandemic:
A
hidden
healthcare
crisis.
Front.
Psychiatry.
2022;
13:
1071397.
doi:
10.3389/fpsyt.2022.1071397
37. Parandeh A, Ashtari S, Rahimi-Bashar F, Gohari-Moghadam K, Vahedian-Azimi A. Prevalence
of burnout among health care workers during coronavirus disease (COVID-19) pandemic: A
systematic review and meta-analysis. Prof Psychol Res Pr. 2022; 53, 564–573. doi:
10.1037/pro0000483
38. Johns, G, Waddington L, Samuel V. Prevalence and predictors of mental health outcomes in
UK doctors and final year medical students during the COVID-19 pandemic. J Affect Disord.
2022; 311, 267–275. doi: 10.1016/j.jad.2022.05.024
39. Pappa S, Sakkas N, Sakka E. A year in review: Sleep dysfunction and psychological distress
in healthcare workers during the COVID-19 pandemic. Sleep Med. 2022; 91, 237–245. doi:
10.1016/j.sleep.2021.07.009
40. Hodkinson A, Zhou, A, Johnson J, Geraghty K, Riley R, Zhou A et al. Associations of
physician burnout with career engagement and quality of patient care: Systematic review
and meta-analysis. BMJ, 2022; 378 :e070442. doi:10.1136/bmj-2022-070442.
41. Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its
consequences: A review. Behav. Sci. 2018, 8; 98. doi: 10.3390/bs8110098
42. Suppapitnarm N, Saengpattrachai M. Physician engagement before and during the COVID-19
pandemic in Thailand. Healthcare, 2022, 10; 1394. doi: 10.3390/healthcare10081394
43. Locke, E. A. The nature and causes of job satisfaction. Handbook of industrial and
organizational psychology. 1976
65